II. Big Pharma
While the CNAS authors wrote their “Predictive Medicine” article before the Covid-19 pandemic, the most prominent institutions in the pandemic preparedness / biosurveillance field have already begun selling the “predictive” approach to public health as the solution to the “next pandemic.” One of the most prominent aspects of predictive health involves using biosurveillance data to fuel the research and distribution of medical countermeasures—a policy that the CDC’s CFA is pursuing:
“[The Analytics Response Branch] works with key partners to inform decisions on medical countermeasures during an active outbreak.”
This policy unsurprisingly has the backing of the industry that most clearly stands to gain the most from it—Big Pharma. In 2023, scientists from Pfizer’s mRNA Commercial Strategy & Innovation department (one of whom hails from John Hopkins Bloomberg School of Public Health) wrote an article titled “Outlook of pandemic preparedness in a post-COVID-19 world” in which they pushed for the utilization of predictive AI technology to inform real-time policy during the “next pandemic.” The scientists pitched AI-informed policy decisions as the solution to the downsides of universal pandemic policies, specifically through a more “targeted” approach to pandemic policy.
The paper advocates for the development of preemptive vaccines, which are vaccines developed for viruses that do not yet spread prominently in human populations. Surveillance data of pathogens with pandemic potential fuels this research, as the paper notes that vaccination benefits have “continued to progress” due to the power of constant biosurveillance and accelerated manufacturing, demonstrated by the development of “updated vaccines for evolving variants of SARS-CoV-2.”
Similarly, the authors tout the abilities of these preemptive vaccines to be quickly dispersed to protect populations from outbreaks of pathogens with pandemic potential if the pathogen “closely aligns” with a preemptively developed vaccine stockpile. These preemptive vaccines, however, would only offer temporary protection until “more tailored interventions” were developed, if deemed necessary.
This echoes the long calls of other global health institutions to develop preemptive vaccines. As a previous Unlimited Hangout investigation reported, the WHO’s 2014 CEPI-partnered program, Research and Development Blueprint for Emerging Pathogens (R&D Blueprint) aims to “reduce the time” that vaccines can get to market after the declaration of a pandemic. It does this, however, not only through conducting R&D on pathogens that already reach pandemic status, but also by conducting R&D on diseases that “are likely to cause epidemics in the future.” CEPI itself—started with investments from the Bill & Melinda Gates Foundation and the Wellcome Trust—was founded to develop “vaccines against known infectious disease threats that could be deployed rapidly to contain outbreaks, before they become global health emergencies.”
CEPI is currently assisting in building up an apparatus of research and private companies pursuing predictive vaccine development, who may up end being some of the “key partners” that the CFA plans to work with to “inform decisions on medical countermeasures during an active outbreak,” given CEPI’s close partnership with the Gates Foundation via the Gates Foundation’s Gavi, the Gates Foundation’s history of funding the CDC and Gates’ potential influence within CFA (demonstrated later in this article). CEPI made these investments to further its “100 Days Mission” that aims to “accelerate the time taken to develop safe, effective, globally accessible vaccines against emerging disease outbreaks to within 100 days.”
Interestingly, CEPI claims that the construction of a “Global Vaccine Library” is crucial to the success of its 100 Days Mission. The Library plans to utilize AI technology to predict how “viral threats could mutate to evade our immune systems” in order to identify specific “vaccine targets.” Richard Hatchett, the CEO of CEPI (formerly of the US Biomedical Advanced Research and Development Authority (BARDA)) stated that building the Global Vaccine Library will require “coordinated investments in countermeasure development and, in outbreak situations, rapid data sharing.” Perhaps the datasets that the CFA will utilize and expand could assist in creating this Global Vaccine Library by making possible the “rapid data sharing” that CEPI requires.

III. Building on Tiberius
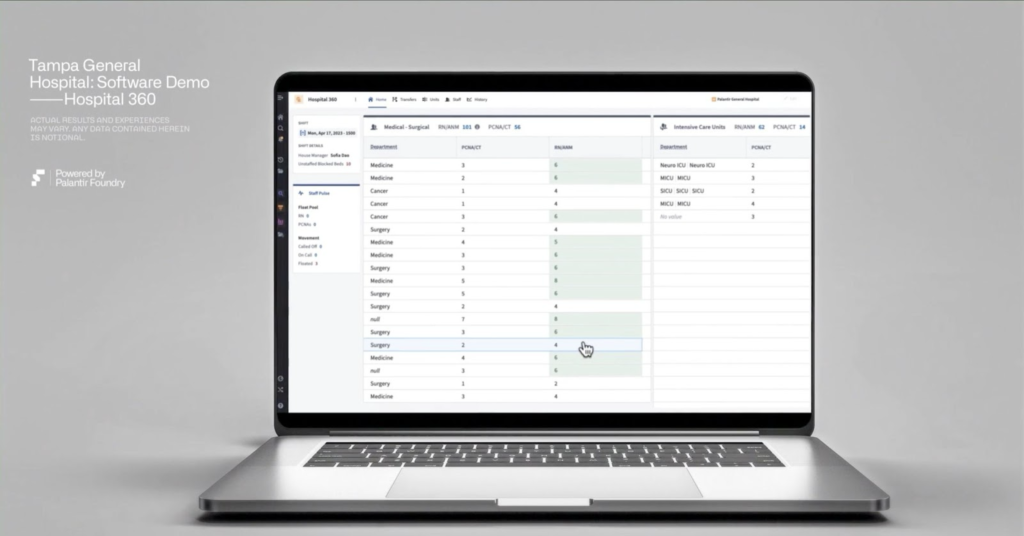
Another element of informing medical countermeasure policy through data is distribution—something that Palantir gained direct experience with during the COVID-19 pandemic. The CFA now plans to utilize its data and analytical tools to inform its “key partners” on “decisions on medical countermeasures during an active outbreak.”
During COVID-19, the Pentagon–run Operation Warp Speed initiated its vaccine distribution policy in direct collaboration with Palantir through the Palantir program “Tiberius,” which the CDC has since pledged to unite with other Palantir biosurveillance programs as part of its “Common Operating Picture.” Tiberius uses a Palantir software product called Gotham that also manages another Palantir-run government program called Health and Human Services (HHS) Protect, “a secretive database that hoards information related to the spread of COVID-19 gathered from ‘more than 225 data sets, including demographic statistics, community-based tests, and a wide range of state-provided data.’” The database notably includes protected health information, which led Democratic senators and representatives to warn of the program’s “serious privacy concerns”:
“Neither HHS nor Palantir has publicly detailed what it plans to do with this PHI, or what privacy safeguards have been put in place, if any. We are concerned that, without any safeguards, data in HHS Protect could be used by other federal agencies in unexpected, unregulated, and potentially harmful ways, such as in the law and immigration enforcement context.”
During the pandemic, Tiberius drew on this health data so that it could “help identify high-priority populations at highest risk of infection.” Tiberius identified the risk levels of these populations in order to develop “[vaccine] delivery timetables and locations” to prioritize vaccines in specific “at risk” populations. Most often these populations were minority communities and notably, the COVID-19 vaccines are associated with an excess risk of serious adverse effects, and can cause fatal myocarditis.
Further, as noted in a previous Unlimited Hangout investigation, intelligence agencies and law enforcement agencies, such as the Los Angeles and New Orleans police departments, also use Gotham for “predictive policing,” or pre-crime initiatives which disproportionately affect minority communities (ICE also used Palantir’s digital profiling tech to apprehend and deport illegal immigrants). The US Army Research Laboratory also found Gotham useful, as evidenced by its $91 million contract with Palantir “‘to accelerate and enhance’ the Army’s research work.” More recently, Palantir teamed up with Microsoft to provide national security leaders with an opportunity to exploit a “first-of-its-kind, integrated suite of technology,” including its Gotham software, among other products, for “mission-planning” purposes (the military also uses Gotham for “targeting enemies” through its “AI-powered kill chain”). These lucrative contracts with the intelligence/military state highlight the dual-use nature of the technology behind the “AI-healthcare” revolution, and thus raise the question: will Palantir and other government agencies utilize the health data that CFA can access for “dual-use,” national security purposes?

The Digitization of Healthcare: Kinsa, Palantir and the ‘Targeted’ Nature of Future Pandemic Response
Notably, some prominent institutions within the biosecurity apparatus have already begun pitching “targeted” pandemic policy as a solution to the now widely recognized failings of the more universal non-pharmaceutical intervention (NPI) policies of COVID-19, such as lockdowns, social distancing and school closures, which unleashed economic devastation, physical death and mental health decline upon many populations.
For instance, the Pfizer paper, “Outlook of pandemic preparedness in a post-COVID-19 world”, mentioned earlier, surmises that the negative effects of NPIs such as school closures, lockdowns and hospital policies may be felt years into the future and even be shown to increase in severity with further studies. Lockdowns in particular, the authors note, “resulted in significant economic, social, and health costs,” and they even state that “the effect of social distancing on the mental health of children and adolescents [continues] to be difficult to measure.” From a bureaucratic perspective, the paper also admits that consistent and long-term use of NPIs can be “challenging because people grow tired and apathetic toward them.”
The solution that the Pfizer scientists offer is “early action” being used to “leverage all available interventions as soon as possible in pandemic response,” and importantly, “geographically specific and informed NPI policies.” It appears that at least one of the solutions the paper puts forth, to both implement “early action” and “geographically specific” policies, is to “have a gradient of warnings that separate dangerous pandemics from more manageable outbreaks…” This proposed policy recalls the CFA measure that analyzes “disease spread through existing data sources to identify key populations/settings at highest risk” (emphasis added).
The paper goes on:
“In healthcare settings, an artificial intelligence platform could help prioritize patients based on their medical needs, effectively managing resources during triage situations. Similarly, a gradient-based warning system for pandemics could initiate appropriate responses at different levels of threat, with each level tied to specific actions. An early warning or Level 1 may involve increased surveillance and information sharing, while higher levels could trigger more drastic measures like regional shutdowns or global travel restrictions.” (emphasis added)
A system of surveillance this vast, importantly, could only be achieved through the “the facilitation and coordination” of all biosurveillance activities—from the local to federal levels of government and healthcare entities— that the CFA will carry out.
Other Pharma-backed organizations have also called for targeted pandemic response policy, such as the Committee to Unleash Prosperity which stated “identifying the most vulnerable groups and focusing resources on their protection will always be critical to any sensible crisis response.” The Committee to Unleash Prosperity is funded by the Pharmaceutical Research and Manufacturers of America, whose members include Pfizer, Johnson & Johnson, Glaxosmithkline, Merck,and Sanofi among other Big Pharma companies. The group was also notably co-founded by Larry Kudlow, formerly one of Trump’s top economic advisors and directors of the National Economic Council during his first term, who—during Covid-19—was part of the group that decided to effectively outsource the U.S. fiscal reponse to the crisis to Larry Fink’s BlackRock.
The push for such “targeted” measures are furthermore indicative of an even greater systemic transformation taking place in the healthcare system. The calls to “help prioritize patients based on their medical needs” in order to “effectively manage resources during triage situations” allude to the industry effort to digitize hospital management, resource allocation and patient care, and, in doing so, expand the health datasets of the biosecurity apparatus. Private companies including Palantir, among others, it turns out, are already playing crucial roles in this AI-hospital revolution.
Meanwhile, the CFA codifies the push towards this AI-system through multiple policies:
“[The Predict Division] assists with tabletop exercises to match policies and resources with forecasts”“[The Office of Management Services] provides direction, strategy, analysis, and operational support in all aspects of human capital management, including workforce and career development and human resources operations”
The first company involved in this shift worth noting is Kinsa Health—a company that “uses internet-connected thermometers to predict the spread of the flu”—which is carrying out the kind of data mining that would enable this kind of predictive and targeted pandemic policy that CFA seeks to carry out. According to the The New York Times, Kinsa is “uniquely positioned to identify unusual clusters of fever because they have years of data for expected flu cases in each ZIP code.” During the COVID-19 pandemic, Kinsa was allegedly able to forecast which locations would become “COVID-19 epicenters” before more traditional surveillance systems could.
The thermometers supply data by connecting “to a cellphone app that instantly transmits their readings to the company.” Interestingly, “Users can also enter other symptoms they feel. The app then gives them general advice on when to seek medical attention.”

In the aftermath of the COVID-19 pandemic, Kinsa has emerged as a rising star within the predictive health industry, as it has secured a significant deal with healthcare company Highmark Health to “predict health care utilization, recognize staffing needs, and plan emergency department and ICU bed capacity when infectious diseases like COVID-19 and influenza spike.” The initiative is “the first health delivery system to utilize Kinsa’s early warning system to model staffing needs and bed capacity”—signifying Kinsa’s increasing role in this healthcare shift.
This preceded health technology company Healthy Together’s 2024 acquisition of Kinsa, which marked a significant step for the thermometer company, as the acquisition signifies the expansion of Kinsa’s predictive powers and datasets into the public sector. The announcement proclaimed that “the synergy between the two companies will empower pharmaceutical companies, healthcare providers, Medicaid agencies, insurance companies, and public health departments with AI-driven tools to proactively respond to and address illness.” The bold vision here is perhaps unsurprising—that is, only when Healthy Together’s peculiar ties to government and Thiel-connected figures, and its larger vision, are understood.
Healthy Together is a Software as a Service (SaaS), or a service that “allows users to connect to and use cloud-based apps over the Internet.” It prides itself on unifying “the objectives of government programs and the needs of residents into a single platform.” The way it does this is through its “One Door” approach, or rather—its mission to make available one’s health records and immunization history “all in one place,” that place being their proprietary app. Indeed, Healthy Together has already partnered with the Department of Veterans Affairs (VA) Lighthouse program to access veteran’s health data ranging from immunization records, “test results, allergy records, clinical vitals, medical conditions and appointment records.” This connectivity was achieved via the VA’s application programming interface (API), as veterans using the Healthy Together app access their medical records through the VA API, which connects different computer programs together. This serves as a small-scale example of the growing harmonization between military and Big Tech data.
In addition to health data, the company also aims to link welfare data and access to its app—a particularly concerning feature given that some US health experts tied to the CIA’s In-Q-Tel and official government Covid-19 response policy previously pitched linking welfare benefits to vaccination status during the Covid-19 crisis.
When Healthy Together partnered with Amazon Web Services (AWS) to join its AWS Partner Network (APN), it created a program that achieves this linkage of welfare data with its app. It was called the “Women, Infants, and Children (WIC) Management Information System (MIS),” or Luna MIS. WIC is a United States Department of Agriculture (USDA) federal assistance program that provides low-income pregnant women and children under the age of five with services such as EBT cards to help them afford food. Luna MIS apparently streamlines “the management of WIC benefits, from application and enrollment to benefit issuance and redemption,” meaning it transfers users’ entire interaction with WIC benefits, from registration to allocation, into the Healthy Together app. The company further supports this “One Door” approach for eligibility, enrollment and recertification for other social programs such as “Medicaid, SNAP, TANF…as well as behavioral health, disease surveillance, vital records, child welfare and more.”
Whether or not data collected via technology such as Kinsa thermometers or health records, such as immunization status, might informs one’s eligibility or enrollment for social programs in the future remains to be seen. Either way, the company already works directly on welfare benefits with the Florida Department of Agriculture and Consumer Services , the Chickasaw Nation in Oklahoma, Missouri Department of Social Services, Maryland Market Money and Maryland Department of Agriculture and more. Given that the company already collects vast amounts of medical data, including vaccination records, linking such data to welfare benefits would likely prove an easy task for the company.
While there is not much public information available about Healthy Together’s board or funding, it appears that the “One Door” service was born out of another app—which is no longer available—called Twenty (as a significant number of Healthy Together’s co-founders/CEOs apparently still work at Twenty, and hold the exact same positions at each company).
According to the Salt Lake Tribune, Healthy Together was developed in the early days of the pandemic when the state of Utah “contracted with mobile app developer Twenty to launch Healthy Together” in order to track the residents of Utah’s “movements” and, for those that fell ill, equip public health workers with a digital contact tracing tool to discover “where they crossed paths with other users.” The Tribune reported that Utah provided Twenty with a $1.75 million contract, along with an additional “$1 million to further develop [Healthy Together].” In other words, Healthy Together was built as a public-private “contact tracing” (i.e. surveillance) app.
Twenty, according to its LinkedIn, was an app that aimed “to drive more human connection” by making it easier for friends to meet up and make plans. It does this, however, by allowing users to see the locations of nearby friends, even cluing them into their friends’ later plans and pinning events for people to meet up at. While Healthy Together and Twenty are separate apps, it appears that the seemingly social location-based tracking technology used for Twenty was swiftly repurposed to create the contact-tracing and health-focused app Healthy Together, as the co-founder and co-CEO of Twenty and Healthy Together, Jared Allgood, stated:
“…at the start of the pandemic, we were contacted by some state governments who are interested in using some of the mobile platform technology that we had built previously, to create a link between the health department and residents in their state…” (emphasis added)
The Salt Lake Tribune explained the contact tracing process that the repurposed technology of Healthy Together helped the state achieve:
“the app uses Bluetooth and location tracing services to record when its users are in close proximity. When a user begins to feel ill, he or she can enter symptoms on the app, which provides directions for testing.”
“State epidemiologist Angela Dunn further explained the process…‘So if you choose to share your data with our contact tracers’ by using the app, she said, ‘they’ll be able to know about the places that you’ve been while you were infectious, and it’ll also provide our contact tracers with a snapshot of other app users who you had significant contact with and potentially exposed with COVID-19 as well’…. ‘that will allow contact tracers to follow up directly with those people and provide them information about how to protect themselves and others,’ she said.”
Now, the goals and functions of Healthy Together seem to have expanded into AI viral forecasting and hospital management with its acquisition of Kinsa, making the private company a potential asset for the CDC CFA, as its experience in working with health data would seemingly make it a fitting “existing data source” for the program.
The people behind these companies too, however, make Kinsa and Healthy Together not too far removed from CFA’s other private sector partners. Healthy Together was funded by SV Angel, the venture capital firm founded by “The Godfather of Silicon Valley,” Ron Conway, who was an early investor in the Elon Musk-and-Peter Thiel-founded Paypal and also in the Peter Thiel-backed Facebook (Thiel and Conway were among the earliest backers of the social network).








